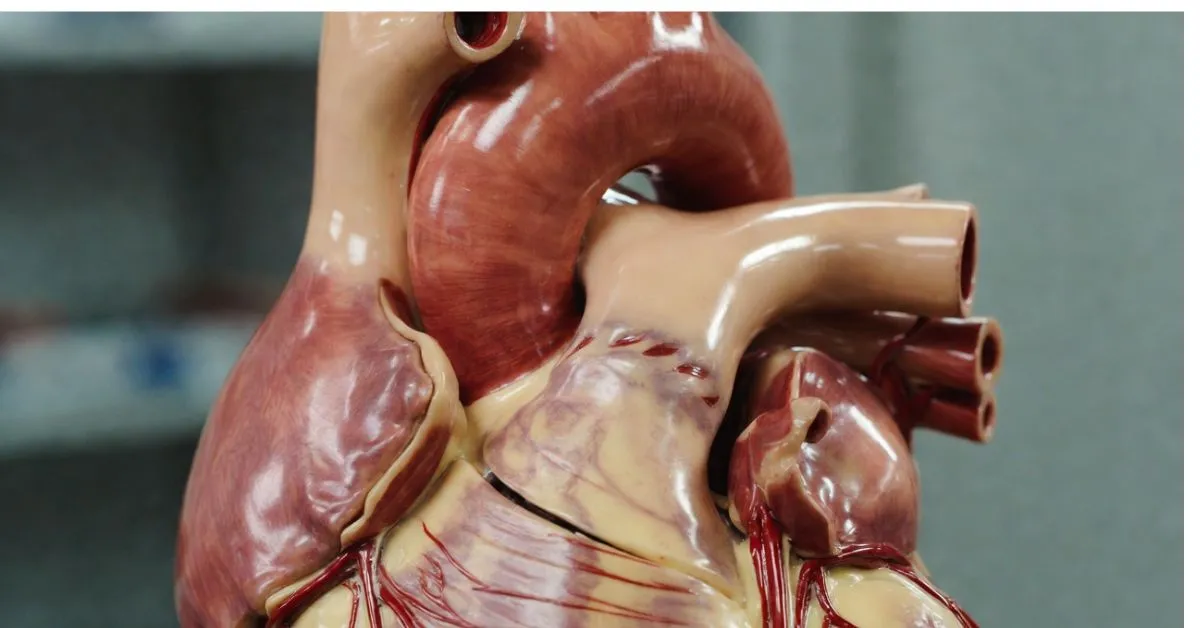
Musculus Papillaris: Tiny Heart Helpers You Never Knew You Needed
Ever stop to think about the small muscles in your heart called musculus papillaris? These papillary muscles make sure your valves close properly with every beat. Come along as we chat about their setup, job, why one is prone to trouble, and how modern checks catch issues early—easy words, no doctor-speak overload.
Hey, your heart’s thumping away this very second—around 100,000 beats today, no breaks, no complaints. Wild, right? For that nonstop pump to send blood the correct direction, the valves between chambers need to slam shut perfectly every time the lower part squeezes. Guess who’s holding those “doors” in place? The musculus papillaris.
People usually just say papillary muscles. They’re these small, cone-like muscle bundles sticking out inside the ventricles (the heart’s main pumping rooms). They don’t get talked about as much as cholesterol or stents, but when one falters, it can turn a bad day into an emergency room nightmare—sudden gasping for air, chest pressure, that scary weak feeling.
Whether you’re prepping for an anatomy exam, helping care for someone post-heart attack, or Googling because a doc dropped the term during a checkup, let’s walk through it together. I’ll keep it straightforward, like telling a friend what I learned.
key Takeaways
- Papillary muscles yank on tough cords (chordae tendineae) to pin heart valves closed during the squeeze—no backflow allowed.
- The posteromedial papillary muscle on the left side usually runs on one artery only, making it 6–12 times more likely to rip after a heart attack.
- Almost a third of hearts have unusual setups—extra muscles, split tips, odd attachments—which can make fixes trickier.
- Fresh imaging tools (strain echo, advanced cardiac MRI) reveal scars, timing glitches, or damage way sooner than basic scans.
- Trouble here worsens things in thick-heart disease (HCM), stretched-heart disease (DCM), and can kick off irregular beats.
Let’s Start Basic: What Is Musculus Papillaris?
It’s Latin for papillary muscles—those nipple-shaped muscle projections inside the ventricles.
Left ventricle (the powerhouse sending blood everywhere) normally has two: anterolateral up front-ish, posteromedial toward the back. Right ventricle usually has three: anterior, posterior, septal.
Each one shoots out strong, stringy chordae tendineae that latch onto the valve flaps (mitral on left, tricuspid on right). Imagine guy-wires steadying a flagpole in a storm—that’s the idea. No slack, no billowing backward.
They form early in fetal life, blending from the same stuff as ventricle walls and valves. Damage anywhere in that group hits the rest hard.
Peeking Closer: Their Build and Surprises
Imagine the left ventricle interior: two pillar-like muscles rise from the walls. Anterolateral sits higher, front-outer area. Posteromedial hangs lower, back near the dividing septum.
Right side: the anterior papillary muscle stands out as the largest, often tied to the moderator band for electrical traffic.
Here’s what throws people—your papillary muscles might not match the textbook picture. Studies find roughly 30% of hearts carry extras: accessory ones, muscles with two or three heads, fused bases, quirky chordae hookups.
Cool variation, sure. But during a valve clip procedure or open-heart repair, an unexpected extra can snag equipment or force a plan change. Chordae layer smartly too—primary to tips, secondary mid-support, tertiary base anchors. Harmony matters.
Blood Flow: The Reason One Side Breaks Easier
Coronary arteries snake over the heart to feed everything. Anterolateral papillary muscle gets two pipelines usually—left anterior descending and circumflex. Block one? The backup keeps it going.
Posteromedial papillary muscle? Often single supply from the posterior descending (right coronary branch in most). One blockage starves it completely.
After infarction, that explains the 6–12× higher rupture rate there. Dead tissue weakens fast under pressure—boom, emergency.
Their Everyday Job in One Beat
Ventricle squeezes hard (systole)—pressure spikes. Without hold-down, valve leaflets flap into the atrium, blood shoots backward, lungs flood, everything crashes.
Papillary muscles contract simultaneously. They shorten, tighten chordae, clamp leaflets flat. They also nudge ventricle geometry for better ejection.
Like adjusting tent stakes just right—not loose (collapse), not over-tight (tear). Balanced pull = one-way traffic.
When It Goes Wrong—and How It Hits Hard
Nightmare version: papillary muscle rupture. Hits 2–7 days post major heart attack. Low odds (0.07–0.26% of MI cases), but huge impact—explains part of sudden post-MI deaths. Valve tears open, massive regurgitation, shock sets in quick.
Posteromedial takes most punishment thanks to single feed. Other triggers: endocarditis chewing tissue, chest trauma, rare spontaneous.
Chronic side: HCM—thick walls + displaced papillary muscles block outflow or mess valve motion. DCM—dilated chamber pulls muscles apart, leaks + fibrosis follow.
Fibrotic zones turn arrhythmogenic—ectopic beats, sustained tachycardia start there.
Today’s Smarter Detection Tools
Basic echo catches leaks, prolapse, gross motion. New layers add power.
Strain echo tracks shortening amount and sync—spots dyssynchrony hidden before. 3D echo visualizes attachments/variants clearly.
Cardiac MRI rules for detail. Late gadolinium enhancement shows old scars; FIDDLE sequences mark acute injury; T1 mapping flags early fibrosis pre-symptoms.
These give precise views—crucial with variant anatomy or subtle changes.
Repair Options and Real Talk on Outcomes
Acute rupture → urgent surgery: reattach muscle or valve replacement. Repair preserves native tissue when feasible; replacement for severe cases. Operative mortality 24–27%; 10-year survival ~35%.
Slower leaks → MitraClip via catheter pinches leaflets. Variant papillary muscles sometimes hinder perfect results or raise complication odds.
Meds stabilize initially: diuretics offload fluid, inotropes support squeeze—bridge to intervention.
Fun Facts & Fresh Directions
Your papillary muscles? Unique as a fingerprint structurally. Recent papers show HCM obstruction often involves them independently of septum thickness. DCM scar burden predicts cardiac mortality strongly.
PET/CT spots active sarcoid involvement here. Arrhythmia ablation from papillary foci improves with better electro-anatomic mapping.
Trend: personalized—map your exact variant first for safer, tailored fixes.
Grasping musculus papillaris highlights heart‘s precise teamwork. Had sudden dyspnea after chest pain? Seen a loved one struggle post-MI? Mention papillary muscles to your cardiologist—pushing for strain echo or MRI can catch brewing issues early, potentially changing the course.
FAQs On Musculus Papillaris
What is musculus papillaris?
It’s the Latin term for Musculus Papillaris muscles—small cone muscles in heart ventricles. They connect to mitral/tricuspid valves via chordae tendineae cords. On each squeeze they pull cords to seal valves, blocking backward blood flow. Slack ones force the heart to overwork.
How many Musculus Papillaris in the left ventricle?
Standard is two: anterolateral (front-side), posteromedial (back-middle). But 30% have variations—extra heads, fusions, accessory ones. That personal twist impacts valve intervention planning a lot.
Why is Musculus Papillaris muscle rupture dangerous?
Sudden tear floods blood backward into lungs—instant congestion, pressure drop, shock. Untreated survival often hours to days. Surgery helps but high risk due to prior damage.
What causes Musculus Papillaris muscle rupture?
Mostly heart attacks starving the muscle (especially posteromedial’s single supply). Also endocarditis, trauma, rare spontaneous. Symptoms erupt days after trigger.
How do doctors diagnose Musculus Papillaris muscle issues?
Echo detects leaks/motion problems first. Strain echo adds contraction timing info. Cardiac MRI best reveals scars, acute damage, early fibrosis via contrast/mapping—great for complex cases.
Can Musculus Papillaris muscles cause rhythm problems?
Yes—fibrosis/scar creates irritable foci for PVCs or tachycardia. Common in DCM. Ablation targets them precisely when meds aren’t controlling.